Some observers outside the pharmacy industry believe that pharmacy benefit managers (PBMs) are a welcome antidote to Big Pharma. As an independent pharmacist, I'd like to share my own perspective on the role PBMs play in the industry.
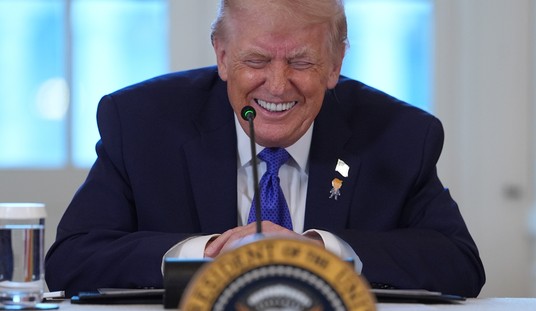
Allow me to speak to you as a former pharmacy owner in the deeply rural Douglas County, Oregon. Douglas County is a rural county which voted 68 percent for Trump in 2020. We were the only pharmacy in the town of 5,000 residents, and the next nearest pharmacy was 12 miles away. I opened this pharmacy after a chain pharmacy pulled out of the market and forced people to drive 20 miles to the nearest chain pharmacy to fill medications. The residents of the town complained they couldn't afford the gas to drive back and forth. Pharmacy options were also incredibly limited, meaning customers would often show up to get their medications only to be told they weren't ready. The reason medications were not ready is multifactorial.
Some chains showed major losses and would end up closing their doors or selling to competitors. As an example, Bi-Mart Pharmacy in Oregon, sold its stores to Walgreens, which closed the existing stores and moved the files to its own stores. Given poor reimbursement, these stores would be managed by one pharmacist at a time, resulting in these patients going days without critical medication, such as insulin, and ending up being admitted to the hospital, costing the healthcare system money that would have been prevented.
Pharmacy benefit managers (PBMs)—the biggest of which are integrated with large health insurers—are the middlemen between insurance companies and health care providers, especially pharmacies. PBMs operate as a middleman and an insurer and also operate their own pharmacies.
PBM regulation is a very popular topic in both red and blue states, with all 50 states having passed some form of regulation against them. There is now conversation to have regulation at the federal level to rein in these conglomerates. PBMs claim to save consumers money, but in reality, what they do is hurt average Americans and cause the cost of healthcare to skyrocket at the expense of profits for themselves.
First of all, CVS Caremark, Express-Scripts, Optum, Humana, and Cigna ranked among the most profitable companies last year in the Fortune 500. Revenue reports show they made 1.25 TRILLION dollars in 2022. The biggest harm they pose currently is under-reimbursing pharmacies on the cost of medications and making a profit on every prescription being billed. The PBMs determine the formulary, that is, the list of drugs they will approve to pay for. Oftentimes, they choose for a plan to use a brand name drug (over the much cheaper generic), and that is determined based on which brand name offers the biggest rebate to the PBM to make it the preferred choice. The PBMs make money from the drug manufacturers, the insurance, and the pharmacy.
The following is a common example of what every pharmacy in America is currently facing:
Drug A costs $500. The pharmacy spends time to type the prescription, check for interactions, fill the medication in a vial with a label, and counsel the patient on it. The pharmacy reasonably expects to be reimbursed above the cost of the medication to keep its doors open. What’s occurring is that the total reimbursement, even with a co-payment, ends up well below the cost of the medication (sometimes a few dollars, sometimes hundreds of dollars) and ensures the pharmacy takes a loss on the medication.
This was the most common result anytime we would bill a brand name medication at my pharmacy, given what the local insurance company would pay at the time. This is the reason I was forced to sell. My store at the time was filling, on average, about 8,000 medications a month. In pharmacy speak, that is an above-average and decent amount of work. The staff was two pharmacists with two or three technicians and a clerk on staff. Due to poor reimbursement, I was unable to make a single profit over two-plus years.
The percentage of loss is very common on brand name prescriptions. Many pharmacies now resort to telling patients they “cannot obtain the medication” because telling the truth can result in the pharmacy losing its contract with the respective PBM. There are no negotiations in these contracts, they are take it or leave it. You accept the poor rates of reimbursement, or you do not get to service the members of that plan. The results of under-reimbursement are now directly responsible for one-third of independent pharmacies closing their doors this year.
What about the chain pharmacies, you may wonder? Low reimbursement impacts them tremendously as well. The chains (although some have their own PBM, they still have to fill medications from rival PBMs) have to cut staff hours, which means overworked and stressed pharmacists, resulting in errors, long wait times for patients to acquire their medications, and hospitalizations. Part of this is in maintaining profits for themselves as well. In doing so, they harm their employees. We have reports of pharmacists like Ashleigh Anderson, only 41 years old, at chain pharmacies who have suffered heart attacks and have died while on the job.
Another practice PBMs participate in is patient steering. It’s anticompetitive, and it’s now outlawed in more than a dozen states. It’s how insurance plans and their PBMs herd patients into pharmacies they own or are affiliated with. As a patient, have you been told, “This pharmacy is out of network,” or “Only allowed one fill and must transfer this medication,” or even “Must use mail order pharmacy”? Or lastly that some co-payments are cheaper with a chain pharmacy owned by the PBM vs the independent pharmacy you want to use?
Patient steering limits patient choices, drives up costs, and puts small pharmacies at a competitive disadvantage. This is most detrimental to rural areas, where, as in our case, the nearest chain store is a long way away, and mail order can take up to seven days to receive an item. Imagine dealing with an infection, high blood pressure, diabetes, or a gout attack and having to wait seven days before getting your prescription. By punishing patients who actively choose their local independent pharmacists with higher costs, PBMs shift money out of the pockets of hardworking Americans into their own corporate coffers. By steering patients to national chains like CVS or to mail-order pharmacies owned by the health insurer-PBM, PBMs drive independent pharmacies out of business, too. And if the practice of manipulating patient choice wasn’t bad enough, PBMs are steering patients to the retail, mail-order, and specialty pharmacies they own.
The practices of PBMs are directly hurting Americans, especially in middle and rural America, where pharmacies are scarce and only getting less prevalent due to the practices of PBMS. If the PBMs have it their way, they will push their competitors out of the market and force everyone to use their own pharmacy (retail or mail order). PBM regulation is not a blue or red issue; it's an American issue that requires immediate fixing. Every patient should have the right to use the pharmacy of their choice, and every pharmacy deserves to make a reasonable profit to be able to continue servicing their patients.
Michel Albert Daher, Pharm. D, APh, is a community pharmacist who has owned and operated three pharmacies located in California and Oregon. He currently owns one in the Los Angeles Area, which specializes in Oncology and long-term care services. He graduated from the Oregon State University/Oregon Health and Sciences University College of Pharmacy in 2013. He completed a one-year residency in ambulatory care at the Old Town Clinic located in Portland, Oregon, where he operated a pharmacy-managed diabetes clinic, which encompassed additional treatment for hypertension, hyperlipidemia, vaccine administration, and heart failure. He is currently an adjunct faculty in the division of pharmacy practice at Marshall B Ketchum University located in Fullerton, Ca. He also holds the title of advanced practice pharmacist, which allows him to prescribe or hold medications and order and interpret lab results.












Join the conversation as a VIP Member