(Editor’s Note: This is a series of articles being published to help people better understand the science behind COVID-19 and the virus which causes it.)
Over the course of the last year, we have had a lot of talk about what COVID-19 isn’t. It isn’t a cold, and it isn’t the flu. But what exactly is it?
SARS-CoV-2 is a virus, same as most other viruses. It is a coronavirus, the same as the common cold, and has symptoms similar to the flu, but aside from that, not much has been known about the virus. Though many in government wanted to freak out about the unknowns of this virus, many didn’t take the time to understand exactly what this virus is, and what exactly this virus does to the body.
From an epidemiological and virological standpoint, SARS-CoV-2 isn’t anything like the flu. From a pragmatic point, they are very similar. To simplify the case even further, comparing sleet and snow would give us a decent comparison. Both are different types of frozen water droplets in the air; however, you’d avoid exposure to them the same way. You’d go inside. You’d drive slower on the roads. You’d put on a coat. You’d turn on your heater at home. You’d salt your walkways.
Similarly, COVID-19 and the flu are different viral pathogens and have different severities, yet, despite the epidemiological and virological differences, the symptoms people suffer, the various treatments deployed, and the populations they affect the most, remain the same. So what made COVID-19 so much worse? Well, to start with, it was a Novel or “new” virus. As a result, medical science had not yet developed a way to block its viral replication. As previously discussed, COVID-19’s infection rate was indeed higher and the effects were certainly and inarguably worse. But why?
To understand this, we must first understand the process of our cellular development. This starts as a portion of the DNA contained in our cells is transcribed or copied into RNA molecules. Those RNA molecules produce mRNA (messenger RNA) or the instructions for cells to produce amino acids which then are then integrated into various types of compounds to produce different proteins. These proteins then feed our body and boost our immune system by feeding T cells, B cells, and antibodies. Cool, huh!?
Hopefully, you’re still following me here.
A viral infection is caused when a virus enters our cells through a process called endocytosis, or the process by which cells “ingest” proteins and compounds which are then broken down to “nourish” the cellular development. The proteins surrounding a virus act as a sort of “trojan horse” and attach to protein receptors on the exterior of our cells. The viral RNA rides, hidden in these proteins, into the cell, and then begins the process of commandeering the cell to reproduce corrupted viral RNA strands and the proteins that surround and protect it.
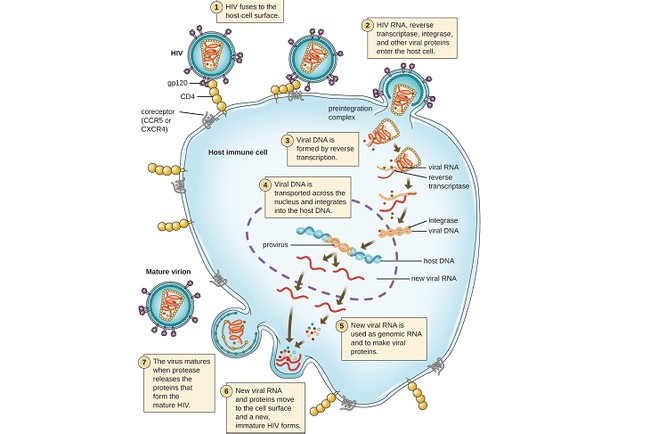
Viruses are everywhere, and many do not infect humans because our protein receptors are incompatible with the proteins surrounding the virus (or the RNA contained therein), thus denying it entry into the cell or the ability to corrupt it to replicate. With viral infections, the virus hijacks our cellular replication process by replacing, reprogramming, or corrupting our cells to produce viral RNA, mRNA, and the proteins necessary in viral replication. Viruses are essentially parasitic, though not actually “alive,” because, unlike bacterial infections, viruses cannot replicate themselves. They require a host cell to create compounds. The corrupted/replicated viral RNA strand is then surrounded by the proteins created by the corrupted mRNA creating virions, or a single viral particle. The cell then expels the virions, or explodes and dies, releasing the replicated virions into our bodies. These replicated virions then repeat the process with surrounding cells, thus spreading the infection.
Both Influenza A and SARS-CoV-2 consist of a single-stranded RNA virus. Both require a specific host for viral replication. However, while Influenza A is a negative-sense RNA virus, SARS-CoV-2 is a positive-sense RNA virus. Negative sense RNA viruses must first create an enzyme which then is used to encode the RNA within the cell to replicate viral RNA (or the virus’s genomic code). That is then used to produce mRNA and subsequently viral proteins which then surround the replicated viral RNA strands creating additional virions. Negative-sense RNA viruses include influenza, ebola, hantavirus, and rabies. Positive-sense RNA viruses are less complicated as they can already act as mRNA, programming cells to produce proteins that then surround the replicated RNA strands, creating new virions. Positive-sense RNA viruses included most coronavirus strains and the common cold.
To summarize the comparison, positive-sense RNA can essentially replace our mRNA in our cells to create virions, while negative-sense RNA either corrupts or works in concert with our mRNA to produce virions.
Previously the SARS-CoV-2 virus has not infected humans as the proteins surrounding the virus or the viral RNA strand contained inside were incompatible with human cells. Our bodies easily determined it to be foreign in the system and it was immediately attacked by white blood cells before any spread of infection could occur. It wasn’t until the virus mutated (through civet cats or potentially engineered in a lab to do so) that it became surrounded by “friendly” recognizable human proteins that allowed it to infect us.
Complicated, I know, but keep following me here.
The reason COVID-19 spread so fast is that the viral replication process for positive-sense RNA viruses (like the common cold) is less complicated than negative-sense RNA viruses (like H1N1). As a positive-sense RNA virus, COVID-19 easily corrupts a cell to reproduce its RNA strand and the mRNA that creates the proteins that protect it. However, that wasn’t the most deadly part about it.
Before we continue, we should review how our immune systems work.
Imagine your town has an expert in bomb disposal. That person knows how to disarm and rid of most bombs and does a fantastic job of keeping the town safe. One day, he’s called to the scene of a new bomb, one he has never seen before. There are two ways this story ends: Either he takes the time to learn how to disarm the bomb before it detonates, or it blows up taking him and the town with it. Occasionally he attends training, learning the new types of bombs, and is even given a chance to practice on some inert and synthesized bombs.
White blood cells in our bodies are the bomb disposal experts. On an average day, those white blood cells identify numerous new threats to your system (viruses, bacteria, dead cells), consume those threats, produce antibodies that neutralize any continued threat, and destroy any particles of and remnants.
Let’s say a virus is introduced into your system. While it begins to infect healthy cells, white blood cells begin a process to rid the body of the viral threat. Some white blood cells, called macrophages, consume these virions before they have the chance to enter and infect other cells. These macrophages present protein and protein fragments to helper T-cells, (another type of white blood cell) which then use these fragments (or antigens) to begin the immune response to destroy infected cells. The helper T-cells take these fragments to B-cells (another type of white blood cell) which uses these fragments to produce antibodies or infection-specific responses to a viral pathogen. Antibodies produced by B-cells attach to infected cells and viruses to prevent them from attaching to the protein receptors of healthy cells and infecting those cells. White blood cells and antigens also help create infection-specific white blood cells called killer T-cells, which can only use their receptors to attach to one type of antigen or protein spike. In this case, the viral antigens and spikes on the exterior of infected cells.
Once the T-cells attach to the antigens or spikes, those cells know it has made contact with an infected cell releasing chemicals to first open the cell and second enter and kill the virus inside. With B-cells creating antibodies preventing the virus from attaching to healthy cells, and killer T-cells attacking already infected cells, the body begins the process of eliminating the viral infection.
Well, why didn’t our immune system immediately recognize SARS-CoV-2 as a threat and eliminate it? That answer takes us further into cellular development (and the case for potential synthetic laboratory development). RNA contains instructions for cells on how to replicate proteins needed for additional cellular development. Encoded into our own RNA is a flag that tells our immune response system to back off that way those cells aren’t attacked. SARS-CoV-2’s RNA contains this piece of code, thus labeling it as harmless to our immune system. Many want to say that this change happened naturally, but the case definitely exists for intentional genomic manipulation.
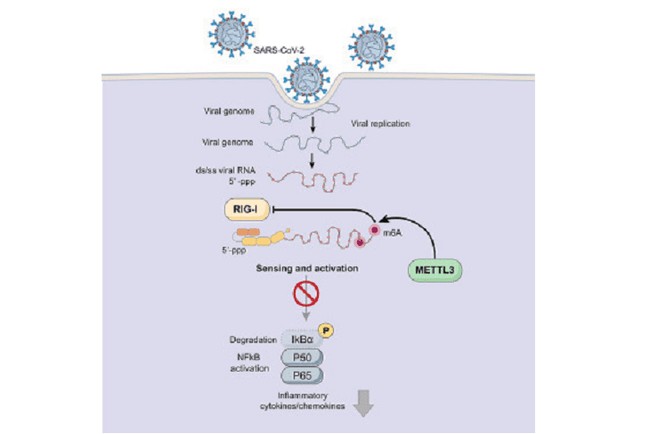
COVID-19 was as severe and deadly as it was because our bodies simply didn’t see it until the resulting infection had already grown to a point of no return. The virus, with help of our cells that had been hijacked, essentially spoofed our body, thus limiting the immune system’s natural response. This perfectly explains why the virus was so severe in those with weakened immune systems.
Tomorrow, we will explore the different types of vaccines and what makes the new Pfizer and Moderna vaccines so interesting.